We all are aware that because of the Covid19 infection and the long lockdown, there has been a very bad impact on both Covid19 positive as well as non-COVID patients. There is more fake news circulating than reliable public health messages. The availability of diagnostics and treatment does not match the needs. With lockdown induced loss of livelihood and reduced access to nutrition, this pandemic is a public health crisis which cannot be managed only with procedures and medicines.
Insurance companies have raised concerns about the high costs being charged by private hospitals. Personal Protective Equipment (PPE) and newer treatment are not covered by private insurance and have to be paid out of pocket by the patient.
During this crisis, we have seen that public health facilities are insufficient and even for a simple lab test, people have to travel all the way to Bangalore from remote parts of Karnataka, worsened by the lockdown of public transport.
Many private hospitals had shut down during the early stages of the lockdown. Now the government is issuing orders and notifications to ensure that private hospitals contribute to healthcare in the State.
In this context, on 20th June 2020, the Government of Karnataka (GoK) had issued an order stating that private hospitals will be empanelled for treatment of Covid19 cases and a notification was issued on 23rd June 2020, fixing the package rate for treatment. These decisions were made by a committee headed by the Executive Director of the Suvarna Arogya Suraksha Trust (SAST) which is managing the health insurance scheme for the State, and after consultation with the Association of Private Hospitals (AHPI), Private Hospitals and Nursing Homes Association (PHANA) and other private hospitals.
On the 25th of June 2020, 28 national and state organisations, challenged the pricing package put out by the GoK for several reasons.
Also Read: The Pandemic and Political imperatives: Rise and Fall of treatment options
First of all, the AHPI is a lobby for large corporate hospitals and has been quite influential in planning and pricing healthcare in Karnataka. The private healthcare sector cannot be the primary decision-maker to plan healthcare or about how taxpayers’ money should be used. The government must make decision-making more consultative, transparent, and public.
One of the clauses in the notification says that in those private hospitals which have the facility to treat COVID 19 patients, 50% beds will be reserved for those referred from public health facilities, and includes High Dependency Units (HDU) and Intensive Care Units (ICU), both with and without a ventilator. The remaining 50% can be used for admitting Covid19 patients privately. The notification doesn’t mention how many beds in each category should be made available. This leaves it up to the hospital to decide what will be given to patients referred from public hospitals and what will be kept for paying patients.
The government will reimburse the costs for patients referred from public hospitals but not for those seeking care privately, although the government has set price caps for both. So, if a COVID positive patient referred from a public hospital is in the ICU with a ventilator, the government will reimburse the hospital Rs. 10,000/day. If the patient has come directly, then for the same treatment, they pay Rs. 25,000/day if they are in general or multi sharing wards. If they are in twin sharing wards, they will be charged an additional 10% and in single rooms an additional 25%. This kind of rules creates different categories of patients, and there will naturally be concerns that some patients (who pay more) may receive better care. When someone is sick, these kinds of difficult choices should not be put before patients.
These fixed package rates also do not cover “unforeseen complications/surgeries/other comorbid conditions/pregnancy etc.” This is highly problematic because the patients who are most at risk in Covid19 are those with comorbidities and may require critical care interventions such as oxygen, ventilator support, high-end medicines, and an extended stay in hospitals. Co-morbidities should be included as part of the package for private patients of Covid19 and the rationale for the treatment option should be documented in detail.
The notification mentions that the fixed rates will not be applicable to patients covered by private insurance or for agreements between the hospital and corporates. Insurance companies have raised concerns about the high costs being charged by private hospitals. Personal Protective Equipment (PPE) and newer treatment are not covered by private insurance and have to be paid out of pocket by the patient. Standard treatment guidelines and price capping should be a protocol applicable for all patients and not based on their ‘package”
AHPI had submitted a “Suggestive Indicative Pricing for treating Covid19 patients” to the Government, with the disclaimer that their suggested costing doesn’t include ‘high end’ drugs and management of co-morbid conditions. This paves the way for irrational and exorbitant billing of patients.

The AHPI has also put out an ‘indicative pricing’ per patient per day for Covid 19 treatment in a general ward. It estimates water, electricity, linen etc. at 500 per day per patient!! This is more than the electricity and water bills that an entire family pays for a whole month! Medication including IV fluids are estimated at Rs. 700 per day per patient. What if the patient doesn’t require medications and just observation? What if the patient is able to take fluids orally? Will they be mandatorily given IV fluids?
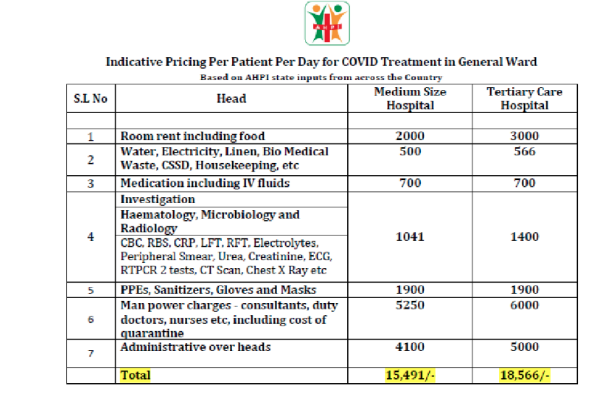
Hematology, microbiology and radiology are estimated at Rs. 1400/day. This is unethical and unscientific practice, and in fact pushes patients to undergo unnecessary tests. Most of these tests are only required at baseline and at occasional intervals to assess progress of disease and response to treatment. If a patient has no respiratory symptoms, what is the need for a chest x-ray and CT scan every day? If the patient has no features of liver disorder, why do liver function tests every day? In any case, many of these tests will not show changes over hours but over days or weeks.
The government should stop the privatisation of healthcare, and instead invest in strengthening public healthcare. This health crisis should be a turning point in India’s health policy making, and bring back the centrality of the public health system in ensuring universal health care.
The writer is a public health doctor and researcher based in Karnataka




























[…] Posted on July 4, 2020 by Dr. Sylvia Karpagam Healthcare during Covid19 – who are the real beneficiaries? […]